Syphilis Is Still Out There – Information for Health Professionals
Syphilis is on the rise in South Australia
It’s essential that during this time we continue to test, treat, cure and notify partners.
Health professionals are now encouraged to have a high clinical suspicion for syphilis in all population groups.
Syphilis Key Points
-
Include syphilis screening as part of a routine STI screen
-
Maintain a high clinical suspicion for syphilis, symptoms of primary and secondary syphilis can include sores, ulcers, rashes, visual changes, hearing issues and alopecia
-
Prevent congenital syphilis risks by regular screening during pregnancy
-
Treatment, contact tracing and follow-up screening at 3, 6 and 12 months is essential to reducing the rates of syphilis infection.
What is Syphilis?
Syphilis is a sexually transmitted infection. It is caused by the spirochete bacterium, Treponema pallidum, subspecies pallidum that can cause serious health problems if left untreated. Syphilis is usually passed on during anal, oral or vaginal sex. It is transmitted through skin-to-skin contact with an infected area. There are four stages of syphilis infection: primary, secondary, latent and tertiary. Each of these stages present different symptoms.
Syphilis is highly infectious during the first two years of infection. Pregnant people can transmit syphilis to their babies, which can result in perinatal death, premature delivery, and congenital abnormalities. Since 2016, South Australia has had five cases of infectious syphilis in pregnant people, and there have been three cases of congenital syphilis. It’s important to know that syphilis also increases the risk of HIV transmission.
Despite the serious health problems associated with syphilis it can be easy to cure if treated early.
Therefore, it is essential that medical practitioners understand the importance of testing and treatment of syphilis as well as the partner/s of those with infectious syphilis.
Symptoms, Treatment and Management

Advice for Health Professionals
Maintain a high clinical suspicion for syphilis in all population groups
- Primary syphilis may present with one or more typically painless ulcers at the site of infection.
- Secondary syphilis may present with a rash and constitutional symptoms such as fever or malaise.
- Be alert to new visual complaints and consider syphilis in the differential diagnosis. Ocular and neurological symptoms may occur at any stage of syphilis.
- Take a dry swab of any potentially syphilitic lesion or rash for syphilis PCR, in addition to bloods for syphilis serology. Herpes simplex (HSV) swabs are unsuitable for syphilis PCR.
Consider syphilis screening in all sexually active patients
- Offer syphilis screening to all asymptomatic patients as part of regular sexual health check-ups. This includes MBS item 715 health assessments for Aboriginal and Torres Strait Islander people.
Request syphilis and HIV serology in patients with other STIs or risk factors for STIs, including STI contacts and persons who inject drugs
- A diagnosis of chlamydia or gonorrhoea indicates that the patient is at risk of syphilis.
- Test for syphilis and HIV in persons diagnosed with or a contact of a person with an STI.
- Offer syphilis screening to persons with evidence of injecting drug use. Injecting drug use is emerging as a behavioural risk factor for syphilis acquisition.
Order syphilis screening early in pregnancy and consider repeat testing
- Ascertain the pregnancy status of all potentially pregnant persons tested for syphilis or other STIs.
- Screen for syphilis at the first antenatal visit. Repeat screening is indicated if the pregnant person or their sexual partner/s are considered at high risk of acquiring STIs, or the risk is uncertain.
- Urgently recall all pregnant persons with reactive syphilis serology to assess the need for treatment.
Facilitate prompt treatment of syphilis and ensure appropriate monitoring
- Treat patients with infectious syphilis promptly with 1.8g/2.4 million units benzathine penicillin (Bicillin L-A) via intramuscular injection (IMI).
- Treat patients with non-infectious syphilis (i.e. asymptomatic infection with no evidence of seroconversion or fourfold rise in reactive plasma regain (RPR) titre in the previous two years) with 1.8g/2.4 million units benzathine penicillin IMI weekly for 3 weeks.
- Treat contacts of syphilis presumptively with 1.8g/2.4 million units benzathine penicillin IMI and collect syphilis serology concurrently.
- Consider ordering benzathine penicillin (Bicillin L-A) through the Emergency Drug Supply Schedule (Prescriber Bag), in order to minimise the risk of treatment delay (https://bit.ly/3jZsBWb).
- Repeat RPR testing at 3, 6, and 12 months to monitor treatment response and exclude re-infection.
Notify new syphilis cases & cases requiring treatment in pregnancy (even if previously notified)
- Notify the Communicable Disease Control Branch
- Download and fax the maroon notification form to (08) 7425 6696.
- Notify by phone on 1300 232 272 if public health advice is required.
Seek advice and assistance from specialist services
- Contact Adelaide Sexual Health Centre for clinical advice on (08) 7117 2800, or CDCB for public health management advice on 1300 232 272, including services through the SA Syphilis Register for Aboriginal and Torres Strait Islander patients.
- See the Australian STI Management Guidelines available at http://www.sti.guidelines.org.au/.
Locating, testing, and treating partners of infectious cases is essential in controlling syphilis.
Syphilis Information and Resources for Health Professionals

Webinar: The Syphilis Surge In South Australia
Presented by SHINE SA GP, Dr Nicola Chynoweth, this 40-minute webinar will discuss the latest information on syphilis and its implications for South Australian health professionals.
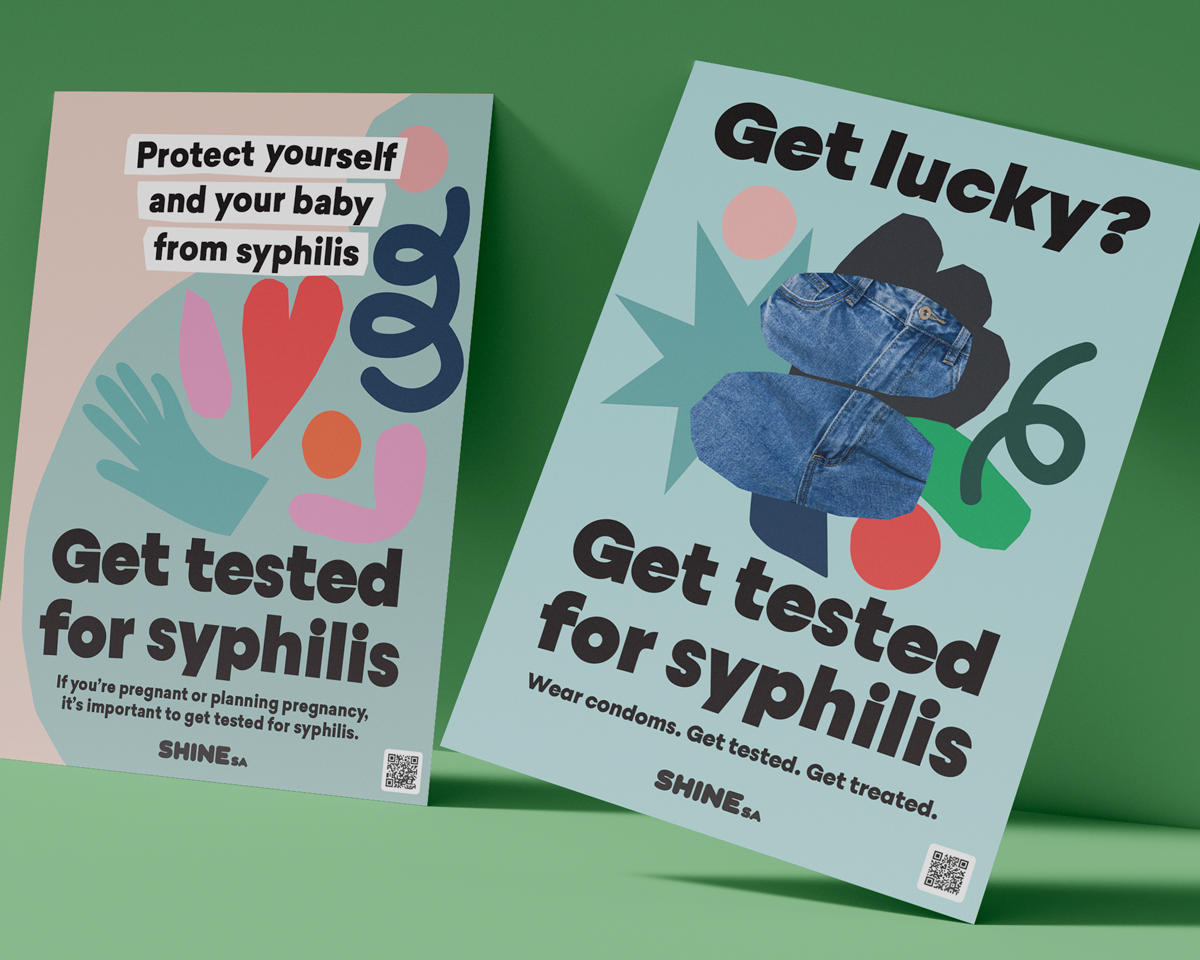
Get Lucky, Get Tested for Syphilis Campaign Resources
Access our Get Lucky, Get Tested for Syphilis Resources
The following organisations can provide advice and guidance around syphilis testing and treatment.
Phone: (08) 7117 2800
Phone: (08) 8300 5300
Aboriginal Health Council of South Australia
220 Franklin Street, Adelaide SA 5000
(Postal address: GPO Box 719 Adelaide SA 5001)
Phone: (08) 8273 7200
Call our Sexual Healthline
The Sexual Healthline is open Monday - Friday, 9:00am - 12:30pm
Country callers: 1800 188 171 (toll-free)